Disclaimer: This guide is written for people who are exploring HELP Apheresis for Long Covid and for clinicians who want to understand the rationale behind our approach.
Living with Long Covid or post‑COVID‑19 condition can feel like being trapped in a body that no longer follows the rules you grew up with. Many of our patients at The Apheresis Center have tried every protocol their Doctors have suggested, yet still find themselves stuck far below their former level of function. For this group of patients, we focus on careful assessment, and in some cases, we use advanced therapies such as therapeutic apheresis that target the biological changes thought to drive ongoing symptoms.
Why Long Covid Often Requires More Than Symptom Management
During our consultations, our patients all tell us a similar story: they rested, paced, followed rehabilitation plans, and tried standard medications, yet their symptoms plateaued or relapsed as soon as they pushed beyond a narrow “safe zone”. In other words, Long Covid behaves less like a short viral illness and more like a chronic relapsing condition with flare cycles triggered by overexertion, infections, heat, or stress.
Clinically, these symptoms and patterns align with the concept of post‑COVID‑19 condition (also called PASC). This is where biological drivers persist even after the initial infection has cleared. Chronic inflammation, autonomic dysfunction, and changes in the vascular system can all contribute to the patient’s feeling of fatigue, brain fog, breathlessness, chest pain, and many other symptoms.
This has profound return‑to‑work implications: even highly motivated people struggle with concentration, stamina, and post‑exertional symptom exacerbation. Despite their best attempts, they find that traditional graded return‑to‑work plans often fail without biological support. We explore this in more detail in our article “Why Long Covid Should Be Treated Like a Chronic Condition”.
What We Currently Know About Long Covid Biology
Whilst research is still evolving around Long Covid, there are several patterns that appear consistently in our patients.
- Persistent inflammation: Long Covid/PASC is associated with ongoing immune activation and elevated inflammatory mediators, which can be present long after the acute infection.
- Endothelial dysfunction: SARS‑CoV‑2 Spike protein can infect endothelial cells and cause endotheliitis, which leads to damage of the blood vessel lining and dysregulation of clotting and blood flow.
- Microclots and impaired microcirculation: Multiple studies have described fibrin amyloid microclots and micro‑thrombosis in acute COVID infection and long COVID, which may obstruct capillaries and reduce oxygen delivery to tissues, causing hypoperfusion.
Kell and colleagues demonstrated that in Long Covid, fibrinogen can form amyloid fibrin microclots that are unusually resistant to normal breakdown. These fibrin amyloid microclots can trap other proteins, including inflammatory molecules and regulators of clot breakdown, potentially sustaining a hypercoagulable state and autoantibody formation.
Jaeger and colleagues reviewed H.E.L.P. (Heparin‑Induced Extracorporeal LDL/Fibrinogen Precipitation) apheresis and highlighted that in COVID‑19, the alveolar tissue and adjacent capillaries often show pro‑coagulant activation, microthrombi, and massive fibrinoid deposits that impair gas exchange.
Taken together, these findings suggest that for at least a subset of patients, Long Covid involves a combination of chronic inflammation, endothelial injury, micro‑thrombosis, platelet aggregation, and impaired microcirculation. We discuss these mechanisms further in“Why You Still Feel Sick: The Hidden Biology of Long Covid”.

Why Blood‑Based Therapies Are Being Studied
If key elements of the pathology are circulating in the bloodstream, such as inflammatory cytokines, abnormal clotting proteins, or microclot‑related material, it is logical to explore extracorporeal therapy that directly modifies the blood.
Therapeutic apheresis is different from medication: rather than adding a drug, it removes selected circulating factors with the aim of improving rheology (blood flow properties), reducing inflammatory load, and supporting endothelial recovery.
The Frontiers in Cardiovascular Medicine review by Jaeger et al. proposes that H.E.L.P. apheresis may benefit acute and long COVID by:
- Removing 50–70% of fibrinogen and reducing plasma viscosity and erythrocyte aggregation, thereby improving microcirculatory blood flow.
- Removing inflammatory cytokines such as interleukin‑6, interleukin‑8, tumour necrosis factor‑α, and C‑reactive protein, which may help to calm the “cytokine storm” and chronic inflammatory state.
- Reducing LDL and lipoprotein(a) can improve endothelial function along with coronary and cerebral perfusion in other vascular conditions.
At the same time, Kell et al. argue that removal or reduction of persistent fibrin amyloid microclots, whether through anticoagulation strategies or other means, may be central to relieving Long Covid-related tissue hypoxia and symptoms. It is important to note that much of this evidence comes from mechanistic studies, observational data, and pilot cohorts rather than large randomised trials, so we avoid framing apheresis as a “cure” and instead present it as an advanced biologically targeted option being actively investigated.
How Therapeutic Apheresis Works
Therapeutic apheresis is a specialized procedure in which your blood is circulated outside the body, where it is filtered and returned to you in a modified form. Conceptually, our patients often find it helpful to think of it as “similar to dialysis,” where blood passes through an extracorporeal circuit, but the goals are different. Dialysis removes waste products in kidney failure, whereas apheresis removes specific plasma components such as lipoproteins, fibrinogen, or immune complexes.
A typical session at The Apheresis Center proceeds as follows:
- Blood is withdrawn via a venous line into the apheresis machine.
- The blood is filtered outside the body, separating plasma from blood cells and selectively removing targeted substances depending on the apheresis method used.
- The processed plasma (sometimes with replacement fluids) and your blood cells are returned to your body through the same circuit.
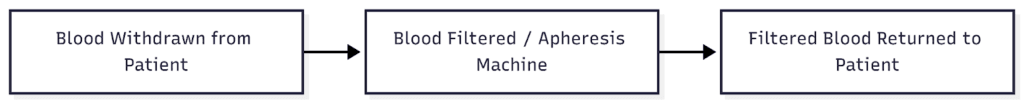
All procedures are performed under specialist supervision with continuous monitoring of vital signs, and treatment plans are individualised based on clinical status, comorbidities, and laboratory parameters.
Types of Apheresis Used in Post‑COVID Conditions
Several different forms of therapeutic apheresis have been applied in COVID‑19 and are now being explored for post‑COVID‑19 conditions:
- H.E.L.P. apheresis is a form of lipid apheresis in which LDL cholesterol, lipoprotein(a), and fibrinogen precipitate at low pH in the presence of heparin and are removed from the plasma.
- Plasmapheresis (plasma exchange), where plasma is removed and replaced with donor plasma or albumin, leads to broader removal of plasma proteins, including antibodies and immune complexes.
At The Apheresis Center, we focus on H.E.L.P. apheresis within our Long Covid and Post-Vac protocols, often as part of our broader “Cyprus Protocol”. This may also include IV therapies, clinical nutrition, health coaching, immunomodulatory therapies, and other supportive treatments.

What HELP Apheresis Targets
H.E.L.P. apheresis was originally designed for severe lipid disorders but has properties that make it a promising candidate in Long Covid and similar post‑viral syndromes. In the extracorporeal circuit, heparin is added, and the plasma pH is lowered to the isoelectric point, where LDL, lipoprotein(a), VLDL, and fibrinogen precipitate and can be removed before the plasma is buffered and returned. In cardiovascular and transplant patients, this has been shown to improve coronary and cerebral blood flow and reduce thrombotic risk.
In a Long Covid context, HELP apheresis is of interest because it can target several factors thought to be relevant:
- Microclots and micro‑thrombosis: By removing fibrinogen and improving rheology, H.E.L.P. may help reduce the burden of fibrin‑rich microclots contributing to capillary blockage.
- Inflammatory mediators: H.E.L.P. apheresis has been shown to remove cytokines such as IL‑6, IL‑8, and TNF‑α, and to reduce C‑reactive protein by more than 50% in some settings.
- Excess lipoproteins: Reducing LDL and lipoprotein(a) can support endothelial health and microvascular perfusion.
- Blood viscosity factors: Lowering fibrinogen and altering the haemorheological profile can reduce blood viscosity and erythrocyte aggregation, improving tissue oxygenation.
When patients search for “HELP apheresis for Long Covid” or “long covid treatment blood filtering”, it is this combination of microclot‑related material, inflammatory mediators, excess lipoproteins, and viscosity factors that we are targeting rather than a vague notion of “detox”.

Potential Benefits Observed in Long Covid Patients
Early observational reports and clinic experiences suggest that selected Long Covid patients may experience symptom improvement after courses of apheresis treatment.
Symptoms commonly reported to improve include the following:
- Fatigue: Increased stamina for daily tasks, reduced post‑exertional crash and malaise.
- Brain fog: Clearer thinking, improved word‑finding, and cognitive processing.
- Exercise intolerance: Better tolerance of walking or gentle exercise with fewer delayed flares.
- Circulation‑related symptoms: Less heaviness, coldness, or colour changes in hands and feet consistent with improved microcirculation.
In the Frontiers review, the authors note that H.E.L.P. apheresis improves myocardial, cerebral, and pulmonary blood flow rates and coronary flow reserve in other conditions, supporting the plausibility of similar benefits where Long Covid symptoms are linked to impaired perfusion. Kell et al. emphasise that removing amyloid fibrin microclots and improving oxygen delivery could mechanistically underpin improvements across multiple symptom domains.
However, it is crucial to be transparent that responses can vary, where some patients experience modest or no benefit, and the long‑term durability of improvements is still being studied. We therefore avoid absolutes or guarantees and stress that apheresis remains one component of a comprehensive Long Covid therapy programme rather than a stand‑alone cure.
HELP Apheresis vs Plasmapheresis for PASC
Key Differences at a Glance
Patients with PASC (post‑acute sequelae of SARS‑CoV‑2) often encounter both “HELP apheresis” and “plasmapheresis” in their research and understandably ask how they differ. The table below summarises key distinctions.
Both are forms of extracorporeal therapy, but they intervene at different levels in the blood and immune system. The choice between them depends on the dominant biology of the patient, for example, microclot‑driven rheology changes or strongly autoantibody‑mediated disease, comorbidities, and individual risk–benefit balance.
| Aspect | HELP apheresis | Plasmapheresis (plasma exchange) |
| Main target | LDL, lipoprotein(a), fibrinogen, lipid-bound inflammatory factors | Broad spectrum of plasma proteins including antibodies, immune complexes, complement |
| Selectivity | More selective; plasma is processed and returned after removal of precipitated components | Less selective; a defined volume of plasma is removed and replaced |
| Key mechanisms in the PASC context | Reduces fibrinogen and viscosity, removes lipid-bound inflammatory mediators, and improves rheology | Removes circulating autoantibodies and immune complexes, modulates the immune response more globally |
| Typical non-COVID indications | Familial hypercholesterolaemia, refractory vascular disease, transplant vasculopathy | Autoimmune neurological disease, antibody-mediated conditions |
| Effect on protective antibodies | Preserves IgM/IgG in standard protocols, according to long-term cardiovascular experience. | Can significantly reduce antibody levels and complement, requiring careful monitoring |
| Use pattern | Often repeated at intervals; Long Covid protocols vary by centre and patient | Usually delivered as a finite series of exchanges over days to weeks |
Why Treatment Choice Matters
Long Covid is not a single disease but a spectrum of presentations that overlap with other immune‑mediated and post‑viral syndromes. Some patients show features suggesting micro‑thrombosis, high fibrinogen, and dyslipidaemia, whereas others have more overt autoimmune features or profound autonomic instability. We also find that many have mixed patterns. For this reason, no single therapy will be suitable or optimal for all patients with PASC.
Apheresis modalities differ in their risk profile, impact on plasma proteins, and logistical demands. Vascular access, procedure duration, anticoagulation, and potential side effects must all be considered alongside likely benefits and the patient’s overall health status.
At The Apheresis Center, we therefore use detailed assessments, not promotional slogans, to decide whether HELP apheresis, other therapies, or conservative management is the safer and more appropriate approach in each case.
Who May Qualify for Therapeutic Apheresis
Common Clinical Patterns Seen in Candidates
Therapeutic apheresis is generally reserved for patients with post‑COVID‑19 condition or Post-Vac Syndrome who have already pursued standard care and remain significantly impaired.
Common patterns we see in candidates include:
- Persistent symptoms > 6 months that substantially limit daily life or ability to work, despite appropriate pacing, rehabilitation, and medical management.
- Poor response to standard care such as symptom‑targeted medications, autonomic rehabilitation, and structured return‑to‑activity plans
- Evidence or strong suspicion of inflammatory or vascular involvement, such as elevated inflammatory markers, hypercoagulability markers, dyslipidaemia, or clinical features consistent with microcirculatory dysfunction.
We also consider overall resilience, comorbidities, and patient goals. For some, the priority may be regaining a few hours of productive energy per day, and for others, it may be returning to professional or caregiving responsibilities. Apheresis is more appropriate when it can be integrated into a realistic, supportive, and sustainable treatment plan.
Who Should Not Undergo Apheresis
Safety exclusions are essential for any advanced procedure. The reasons why someone may not be a suitable candidate for therapeutic apheresis include:
- Bleeding disorders: Severe coagulation abnormalities that make anticoagulation unsafe or greatly increase bleeding risk.
- Unstable cardiovascular conditions: Such as uncontrolled arrhythmias, decompensated heart failure, or recent major cardiac events.
- Contraindications identified during screening: Severe anaemia, uncontrolled infection, inability to achieve safe vascular access, or allergic risk to components of the circuit or replacement fluids.
In some cases, these issues can be optimised first, in others, we may advise against apheresis and instead focus on safer strategies. If you are not a candidate for apheresis, that is not a judgment on the reality or severity of your symptoms, but instead it reflects our responsibility to avoid exposing you to procedures where the risks outweigh likely benefits.
Risks vs Benefits of Therapeutic Apheresis in Long Covid
Potential Benefits
Potential benefits of apheresis treatment for Long Covid when delivered in carefully selected patients include:
- Symptom relief in selected patients: Particularly in fatigue, cognitive clarity, exercise tolerance, and circulation‑related symptoms.
- Improvements in circulation markers: Rheological parameters, such as reductions in fibrinogen, plasma viscosity, and certain inflammatory markers, which may support better tissue oxygenation.
In cardiovascular cohorts, H.E.L.P. apheresis has been associated with improved myocardial and cerebral blood flow and reduced thrombotic events. This supports the broader concept of using rheology‑modifying therapy in vascular‑inflammatory conditions. In Long Covid, we are still learning how best to translate these physiological effects into lasting functional gains.
Known Risks and Limitations
Apheresis is an invasive and resource‑intensive therapy. Known risks include:
- Vascular access complications: Bruising, bleeding, thrombosis, or infection at access sites.
- Transient side effects: Light‑headedness, fatigue, blood pressure changes, and electrolyte shifts during or after treatment.
- Plasma‑related reactions: In plasma exchange (less relevant for HELP), allergic or anaphylactic reactions to donor plasma or replacement fluids.
From an evidence standpoint, the limitations include:
- Limited large‑scale trial data: Most current evidence for apheresis in Long Covid comes from mechanistic studies, case series, and early cohorts, rather than large randomised controlled trials.
- Variable response: Not all patients improve, and the degree and durability of benefit can differ markedly.
- Access and cost considerations: These treatments may not be widely available or covered by all health systems.
For these reasons, we emphasise that therapeutic apheresis for Long Covid is still an evolving area of medicine, with ongoing research needed to refine patient selection, protocols, and long‑term outcomes.
Is Apheresis the “Latest Treatment” for Long Covid?
Our patients often ask whether apheresis is the “latest” or “best” Long Covid treatment. The honest answer is that there is no single latest or universal treatment that works for everyone with post‑COVID‑19 condition. Long Covid is biologically and clinically diverse, and what helps one person may not help another.
Apheresis is one advanced option under investigation for a specific subset of patients who appear to have significant vascular‑inflammatory involvement and have not improved sufficiently with standard care. It should ideally sit within a broader care plan that addresses autonomic dysfunction, sleep, mental health, rehabilitation, nutrition, and pacing strategies, rather than being viewed as a stand‑alone solution.
We discuss symptom‑management strategies such as pacing, heat management, and daily living adaptations in more detail in our Long Covid resources and in “Managing Long Covid Heat Intolerance in the Heat of Summer”.

A Comprehensive, Individualised Treatment Approach
At The Apheresis Center, we do not start with apheresis; we start with you. Every patient begins with a detailed consultation that covers symptom history, triggers, relapses, medical background, and previous investigations.
We use structured symptom mapping to understand patterns such as post‑exertional malaise, orthostatic intolerance, temperature sensitivity, sleep disruption, and cognitive fluctuations, because these often reflect underlying biology.
Laboratory review may include markers of inflammation, coagulation, lipids, autonomic and endocrine function, and other relevant tests depending on your presentation.
Based on this, we discuss options that may include:
- Long Covid education;
- Pacing strategies;
- Clinical nutrition;
- Health coaching;
- IV therapies and other supportive treatments.
- H.E.L.P. apheresis and combination protocols where appropriate.
Crucially, we use a shared decision‑making approach where we discuss the evidence, the uncertainties, the risks, and the likely commitments involved. We decide together whether apheresis is a good fit for your goals and situation. For a broader overview of our approach, see our Long Covid pillar page.
Storie di successo e testimonianze
Many patients from across the globe, including the USA, Australia, Europe, and the UK, have experienced significant improvement through our Long COVID Therapy treatment protocols. Their success stories are a testament to the efficacy of our approach.
Patient Questions We Hear Most Often
Does apheresis help Long Covid patients?
Some Long Covid patients report meaningful improvement in symptoms such as fatigue, brain fog, exercise tolerance, and circulation‑related complaints after one or more apheresis treatments, particularly when there is evidence of microclot‑ and inflammation‑driven pathology.
However, responses vary, not everyone benefits, and we cannot promise specific outcomes for any individual.
How is HELP apheresis different from plasma exchange?
HELP apheresis selectively removes LDL, lipoprotein(a), fibrinogen, and certain inflammatory mediators while largely preserving protective antibodies. Plasma exchange removes a broader range of plasma proteins, including antibodies and complement, and replaces them with donor plasma or albumin, making it more suitable for strongly autoantibody‑mediated diseases but also more disruptive to the immune milieu.
How many sessions are usually considered?
The number and timing of sessions depend on your individual clinical picture, your lab results, your response to initial treatments, and overall goals. Some patients undergo a short, intensive block while others receive more spaced‑out treatments combined with rehabilitation and other therapies. There is no one‑size‑fits‑all protocol, and we review progress regularly.
Can Long Covid be fully reversed?
There are patients who recover substantially or even feel “back to baseline” over time with or without advanced interventions. However, we do not claim that apheresis or any other single treatment can fully reverse Long Covid in every case. Our focus is on improving function, reducing symptom burden, and supporting long‑term health in an honest, realistic way.
Is apheresis suitable for ME/CFS‑like symptoms?
Long Covid overlaps with ME/CFS and other post‑viral syndromes, particularly where there is post‑exertional malaise, autonomic dysfunction, and cognitive impairment. Apheresis may be considered where there is strong evidence of vascular‑inflammatory involvement and microclot‑related pathology, but it is not routinely indicated for all ME/CFS‑like presentations and requires careful individual assessment.
What happens if I’m not a candidate?
If apheresis is not appropriate or safe for you, we will explain why and focus on other ways to support you, including symptom‑focused care, pacing strategies, autonomic rehabilitation, nutritional support, and coordination with your local medical team. Being ineligible for apheresis is not a reflection of whether you “deserve” treatment, but a medical decision to protect you from disproportionate risk.
Credibility, Disclaimers, and Next Steps
This article reflects the experience and research focus of The Apheresis Center, which provides H.E.L.P. apheresis and combination therapies for Long Covid, Post Vac Syndrome, and related chronic conditions. It is based on peer‑reviewed studies, including reviews on H.E.L.P. apheresis in COVID‑19 and on amyloid fibrin microclots in Long Covid, as well as our clinical protocols.
Medical disclaimer
This content is for informational purposes only and does not replace personalised medical advice. Diagnostic and treatment decisions must be made in consultation with a qualified healthcare professional who understands your full medical history.
If you recognise yourself in the patterns described here and are seeking a targeted, biology‑informed approach, you can learn more about our comprehensive Long Covid Therapy programme and book an initial consultation through our website.
Author / Medical Review Note
Written by Andrew Smith. Reviewed by Dr Inbar Tofan, Medical Director at The Apheresis Centre. Dr Inbar has over 10 years of clinical experience in internal medicine and therapeutic apheresis, specialising in chronic inflammatory and auto-immune conditions.
Risorse scientifiche e ulteriori letture
I nostri protocolli di trattamento sono basati su una rigorosa ricerca scientifica. Ecco alcune risorse chiave per chi è interessato alla scienza alla base delle nostre terapie:
Study on Microclots, Hypercoagulation and H.E.L.P. Apheresis in Long COVID: https://apheresiscenter.eu/combination-therapy#studies
Research on H.E.L.P. Apheresis: https://apheresiscenter.eu/h-e-l-p-apheresis
Combination Therapy Benefits: https://apheresiscenter.eu/combination-therapy
The potential of heparin-induced extracorporeal LDL/fibrinogen precipitation (H.E.L.P.)-apheresis for patients with severe acute or chronic COVID-19 (https://pmc.ncbi.nlm.nih.gov/articles/PMC9592739/)
A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications (https://pmc.ncbi.nlm.nih.gov/articles/PMC8883497/)